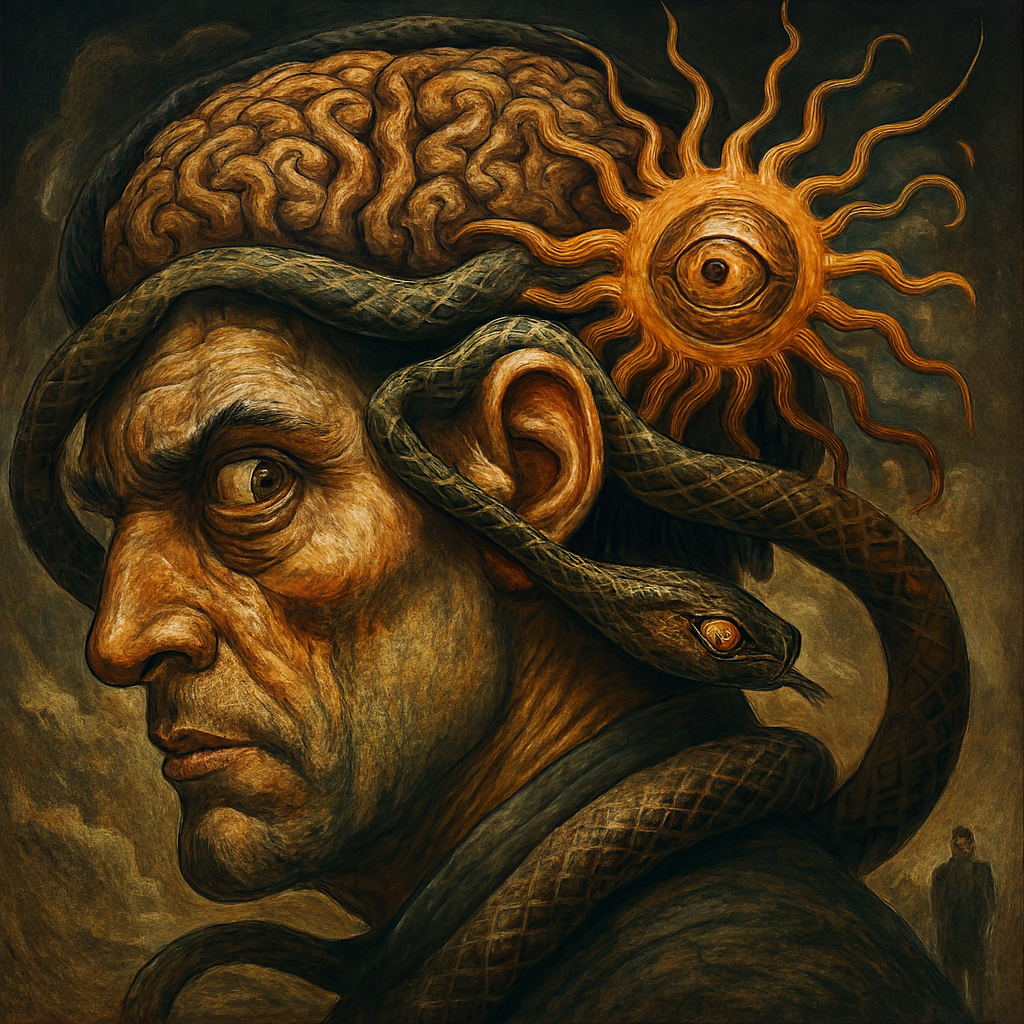
The Strange Paranoid Psychology Of A Paranoia Mind
How Paranoia Alters Brain Function and Emotional Processing The Hidden Costs of Living in a State of Constant Threat
Mapping the Neurobiology, Psychology, and Social Fallout of Chronic Suspicion
Paranoid Psychology
Paranoia is a persistent mental state characterized by irrational suspicion and mistrust of others. It is distinct from general anxiety because it involves specific beliefs about intentional harm or betrayal. Clinical studies show that paranoia can occur in both psychiatric conditions and high-stress environments. It is commonly associated with schizophrenia, delusional disorder, and borderline personality disorder. However, subclinical paranoia also affects individuals without formal diagnoses.
Neuroimaging reveals that paranoid individuals exhibit heightened activity in the amygdala, which processes fear. Dopamine dysregulation plays a key role in assigning undue significance to neutral stimuli. This leads to misinterpretation of social cues and environmental signals. Chronic paranoia can impair decision-making, emotional regulation, and interpersonal relationships. Understanding its mechanisms is essential for both clinical treatment and public awareness.
Neurochemical Shifts in the Paranoid Brain
Paranoia is linked to increased dopamine transmission in the mesolimbic pathway. This pathway is responsible for reward processing and salience attribution. When dopamine levels rise abnormally, individuals may perceive neutral events as personally significant. This phenomenon is known as aberrant salience. Functional MRI scans show that the amygdala becomes hyperactive during paranoid episodes. The prefrontal cortex, which governs rational thought, often shows reduced connectivity. This imbalance between emotional reactivity and cognitive control contributes to distorted thinking. Elevated cortisol levels indicate chronic stress in paranoid individuals. Over time, these neurochemical changes can become entrenched through neuroplasticity. Paranoia is not merely psychological—it reflects measurable changes in brain function. These findings support the need for integrated medical and psychological interventions.
The Fear Response Of Constant Threat
Cognitive Distortions and Thought Patterns
Paranoid thinking involves several well-documented cognitive distortions. Personalization causes individuals to interpret unrelated events as targeted attacks. Catastrophizing exaggerates the consequences of perceived threats. Confirmation bias leads individuals to seek evidence that supports their fears. These distortions are automatic and often resistant to logic or reassurance. Hypermentalizing is another feature, involving over-interpretation of others’ intentions. Paranoid individuals may misread facial expressions or tone of voice as hostile. These thought patterns create a feedback loop that reinforces suspicion. Cognitive behavioral therapy aims to disrupt these distortions through structured reframing. Without intervention, these patterns can become chronic and debilitating. Recognizing them is the first step toward restoring cognitive clarity.

Emotional Volatility
Emotional Dysregulation and Fear Response
Paranoia heightens emotional sensitivity to perceived threats. Individuals often experience intense fear, anger, or sadness in response to minor cues. This emotional volatility can strain relationships and increase social withdrawal. The fear response is disproportionate and persistent, even in safe environments. Sleep disturbances are common due to hypervigilance and racing thoughts. Appetite and energy levels may fluctuate, contributing to physical health decline. Chronic stress from paranoia can lead to burnout and depressive symptoms. Emotional regulation strategies such as mindfulness can help restore balance. Dialectical behavior therapy is also effective in managing emotional extremes. Emotional dysregulation is not a character flaw—it is a symptom of neuropsychological disruption.
Social Isolation and Relationship Breakdown
Paranoia erodes trust and damages interpersonal relationships. Individuals may accuse loved ones of betrayal without evidence. This leads to conflict, withdrawal, and eventual isolation. Social isolation reinforces paranoid beliefs by removing corrective feedback. Studies show that loneliness increases susceptibility to paranoid ideation. Lack of social support can exacerbate emotional distress and cognitive distortions. Paranoid individuals may avoid social situations to prevent perceived threats. This avoidance behavior limits opportunities for reality testing. Over time, isolation becomes both a cause and consequence of paranoia. Rebuilding trust requires consistent, nonjudgmental support from others.
Impact on Occupational Functioning
Paranoia can significantly impair workplace performance. Suspicion toward colleagues may lead to conflict and reduced collaboration. Individuals may misinterpret feedback as criticism or sabotage. This can result in defensive behavior and poor communication. Chronic stress affects concentration, memory, and decision-making. Paranoid employees may struggle with authority figures or team dynamics. Absenteeism and job turnover are common outcomes. Occupational therapists often address paranoia through structured routines and coping strategies. Supportive work environments can mitigate some of these effects. Employers should be educated about mental health to reduce stigma. Early intervention improves long-term occupational outcomes.

Paranoia in Trauma Survivors
Trauma is a major risk factor for developing paranoid ideation. Survivors of abuse, violence, or betrayal may develop hypervigilance. This is a protective mechanism that becomes maladaptive over time. Post-traumatic stress disorder often includes paranoid symptoms. Flashbacks and intrusive thoughts can reinforce feelings of threat. Trust issues are common among trauma survivors with paranoia. Therapy must address both the trauma and the resulting cognitive distortions. Eye Movement Desensitization and Reprocessing (EMDR) is one effective approach. Trauma-informed care emphasizes safety, empowerment, and collaboration. Healing requires validation of the survivor’s experience. Paranoia in this context is a response to real harm, not delusion.
Cultural and Environmental Influences
Paranoia is shaped by cultural and environmental factors. Societies with high levels of surveillance or authoritarian control may foster suspicion. Marginalized groups often experience systemic discrimination, fueling mistrust. Cultural beliefs about privacy, honor, or betrayal influence paranoid thinking. Environmental stressors such as poverty or violence increase vulnerability. Media exposure to conspiracy theories can exacerbate paranoia. Social fragmentation and lack of community support are contributing factors. Cross-cultural studies show variation in how paranoia is expressed and interpreted. Clinicians must consider cultural context when diagnosing and treating paranoia. Environmental interventions can reduce stress and improve mental health. Paranoia is not isolated—it reflects broader social dynamics.
Paranoia in Digital Spaces
Online environments can amplify paranoid ideation. Social media algorithms often reinforce confirmation bias. Individuals may interpret online interactions as surveillance or targeting. Cyberbullying and doxxing contribute to digital paranoia. Privacy breaches and data tracking increase feelings of vulnerability. Virtual communication lacks nonverbal cues, leading to misinterpretation. Paranoid individuals may obsessively monitor others’ online behavior. Digital detox and media literacy are recommended interventions. Therapists increasingly address online paranoia in clinical settings. The internet is both a trigger and a mirror for paranoid thinking. Responsible digital design can help reduce psychological harm.
Sleep Disruption and Circadian Impact
Paranoia disrupts sleep patterns and circadian rhythms. Hypervigilance makes it difficult to fall or stay asleep. Nighttime is often associated with increased fear and rumination. Sleep deprivation worsens emotional regulation and cognitive function. Insomnia is a common complaint among paranoid individuals. Melatonin production may be suppressed due to chronic stress. Poor sleep contributes to irritability and reduced coping capacity. Sleep hygiene practices can improve rest and reduce paranoia. Cognitive behavioral therapy for insomnia (CBT-I) is effective. Restoring sleep is essential for overall mental health.
Physical Health Consequences
Paranoia affects physical health through chronic stress. Paranoid individuals may neglect medical care due to mistrust. This can lead to untreated conditions and worsening health. Mind-body interventions such as yoga or tai chi may help. Regular exercise reduces stress and improves mood. Physical health must be addressed alongside psychological treatment.

Paranoia in Adolescents and Young Adults
Adolescence is a vulnerable period for developing paranoid ideation. Identity formation and peer dynamics contribute to social sensitivity. Bullying and exclusion can trigger mistrust and fear. Early signs include withdrawal, irritability, and academic decline. Young adults may struggle with autonomy and perceived judgment. Substance use can exacerbate paranoid symptoms. Early intervention improves prognosis and prevents escalation. School counselors and youth programs play a critical role. Family support and open communication are protective factors. Paranoia in youth requires age-appropriate, empathetic care.
Diagnostic Criteria and Clinical Assessment
Paranoia is assessed using structured clinical interviews and psychological tests. The DSM-5 includes paranoid personality disorder and delusional disorder. Clinicians evaluate the intensity, duration, and impact of suspicious thoughts. Differential diagnosis is important to rule out other conditions. Assessment tools include the Paranoia Scale and PANSS. Cultural sensitivity is essential during evaluation. Co-occurring disorders such as depression or PTSD are common. Accurate diagnosis guides appropriate treatment planning. Clinical judgment must balance empathy with objectivity. Diagnosis is the foundation for effective care.
Treatment Modalities and Recovery Pathways
Paranoia is treatable through a combination of therapies. Cognitive behavioral therapy addresses distorted thinking. Antipsychotic medications may be prescribed in severe cases. Mindfulness and stress reduction techniques improve emotional regulation. Peer support groups offer validation and shared experience. Trauma-informed therapy is essential for survivors. Recovery is gradual and requires consistent effort. Therapeutic alliance is a key predictor of success. Family education reduces conflict and improves outcomes. Holistic approaches consider physical, emotional, and social factors. Treatment must be individualized and adaptive.
Conclusion
Paranoia is not a fringe phenomenon—it is a deeply rooted psychological and neurological condition that affects millions across diverse contexts. Its impact spans cognition, emotion, relationships, physical health, and occupational functioning. Scientific research confirms that paranoia involves measurable changes in brain chemistry, especially in dopamine regulation and amygdala activity. Cognitive distortions such as personalization and confirmation bias reinforce the cycle of suspicion.
Emotional dysregulation and chronic stress further entrench the condition, often leading to social isolation and physical decline. Cultural, environmental, and digital factors can amplify paranoid ideation, making it more pervasive and harder to detect. Early intervention through therapy, education, and community support can significantly improve outcomes. Recovery is possible, but it requires sustained effort and compassionate care. Paranoia should be understood not as a flaw but as a signal—one that calls for deeper inquiry, healing, and systemic awareness. By mapping its mechanisms and consequences, we move closer to empathy, clarity, and transformation.
Join the Discussion
Have you encountered paranoia in your personal or professional life? What strategies have helped you or others navigate its challenges?
#MentalHealthAwareness #NeurobiologyOfParanoia #CognitiveDistortions #EmotionalRegulation #TraumaRecovery #SocialIsolation #DigitalPsychology #SleepAndMentalHealth #YouthMentalHealth #CulturalContextMatters #OccupationalWellbeing #ParanoiaAndHealing #MindBodyConnection #TherapeuticIntervention #PsychologicalSafety